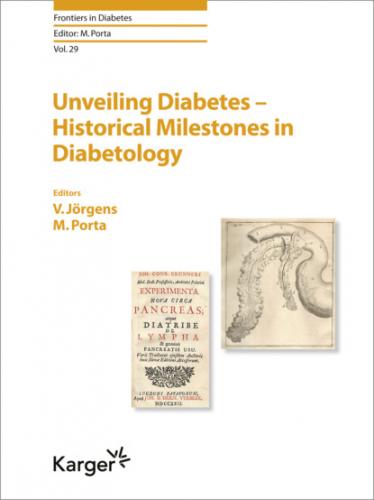
Fig. 10. Frontispiece and illustration of pancreatectomy in Joseph Conrad Brunner’s Experimenta nova circa Pancreas atque Diatribe de Lympha and genuine Pancreatis Usu. London, 1722. The Museum of Diabetes, Turin. www.museodeldiabete.it. Reprinted with kind permission.
Of interest, in 1788, is a report by Thomas Cawley, chief surgeon of the British Army in Jamaica, of a hardened pancreatic gland, embedded with calculi, at the postmortem of a person affected by diabetes. At any rate, he continued to ascribe diabetes to the “morbid dilatation of the uriniferous tubes” [25].
However, not all patients with diabetes had the same characteristics and, importantly, the same prognosis. Apollinaire Bouchardat (1806–1886), professor of hygiene and chief pharmacist at the Hôtel-Dieu in Paris, compiler of the official Formulaire for the French Ministry of Health, started to distinguish a “diabète maigre” in individuals young, lean, with severe symptoms and a poor outcome, from a “diabète gras” in those overweight in whom a milder form of disease presented later in life and who could survive longer on a low-calorie diet. Bouchardat suggested as first measure the suppression of bread and almost all other carbohydrates but conceded their partial reintroduction after the disappearance of glycosuria, which the patients could detect alone by tasting their own urine, a first in patient self-management. Bouchardat’s regime also included abundant amounts of protein and fat, a good bottle of red wine a day, days of complete fasting, avoidance of anger, and vigorous exercise in the open air [26, 27].
Arnaldo Cantani (1837–1893), director of Medicine at Naples University and the first Italian diabetologist, prescribed true starvation diets, albeit “fat and rich in meat,” and it seems he used to lock the poor glycosuric patients in, so that they would not transgress [28]. In 1869 the 22-year-old German medical student Paul Langerhans (1847–1888) described in his doctoral thesis the presence of small agglomerations or “islands” of cells in the pancreas, with characteristics which differed from those of the rest of the organ [29]. Of course, he was unaware that what would come to be known as “islands of Langerhans” produced insulin and, indeed, never knew that he had opened a seminal chapter in medicine and never dealt with diabetes in the remainder of his short life [see the chapter by Jörgens; this vol., pp. 25–35].
Twenty years later, in 1889, the story of Brunner repeated itself in the University clinic of Strasbourg directed by Bernhard Naunyn (1839–1925), himself interested in the problems of metabolism. In 1889, Joseph von Mering (1849–1908) and Oskar Minkowski (1858–1931) were studying the role of the pancreas in digestion and removed the organ from a dog. Again, all the symptoms of diabetes appeared after the operation. This time, however, Minkowski, who had carried out the surgery, rushed to analyze the dog’s urine and found glucose in large quantities. He then repeated the operation in other animals with the same result and concluded that the pancreas produces some substance capable of decomposing the sugar in the blood, in the absence of which diabetes appears [see the chapter by Jörgens; this vol., pp. 40–50] [30].
After Minkowski’s discovery, researchers attempted to extract from the pancreas the mysterious agent that could cure diabetes. Minkowski himself, in 1890, grafted fresh pancreatic fragments under the skin of another diabetic dog, temporarily reducing glycosuria. In 1893, the French Gustave-Édouard Laguesse (1861–1927) suggested that the islands of pancreatic tissue described by Langerhans might be the source of the substance involved in blood glucose control [31]. Among others, in 1893, Ferdinando Battistini (1867–1920) in Turin injected an aqueous-glyceric extract of bovine pancreas into 2 young patients for a few days, albeit without modifying the course of their diabetes [32]. Like the grafts, pancreatic extracts, obtained with various methods, proved ineffective, toxic, or both.
During the following 30 years more evidence accumulated that the elusive antidiabetic factor came from the islands. The name “insulin,” from the Latin “insulae,” was proposed in 1909 by the Belgian Jean de Mayer (1878–1934) and in 1910 by the Englishman Sir Edward Albert Sharpey-Schafer. In 1909, the Berliner Georg Ludwig Zülzer (1870–1949) [see the chapter by Jörgens; this vol., pp. 58–72] came close to the solution by producing an alcoholic extract of bovine pancreas (Acomatol) but this proved toxic at first and then induced seizures in dogs, possibly due to severe hypoglycemia [33]. In 1916, Nicolas Constantin Paulescu (1869–1931), professor of physiology in Bucharest, injected diabetic dogs with an aqueous pancreatic extract, reducing their blood glucose and causing death in some due to hypoglycemia, but the results were not published until 1921 [34, and the chapter by Jörgens; this vol. pp. 58–72].
References
1Barbero PL, Bruni B: Storia del trattamento del diabete. Turin, Centro di Diabetologia Karen Bruni Bøcher, 1979, pp 1–291.
2The Ames Collection. Elkhart, Miles Laboratories, 1985.
3Charaka-Samitha: Charakasamitha. Jibananda Vidyasagara (ed). Kolkata, Sararvati, 1877.
4Sushruta Samitha; Sushruta Samitha. Kolkata, Jibananda Vidyasagara, 1909.
5Bruni B: Storia breve del diabete mellito. Turin, Museo del Diabete Karen Bruni, 1997, pp 1–92.
6Celsus AC: De medicina libri octo. Florence, Nicolaus, 1478.
7Rufus of Ephesus: Oeuvres (by Daremberg C, Ruelle CF). Paris, Impr Nationale, 1879.
8Aretaei Cappadocis: Medici insigni ac vetustissimi. Libri septem. A Iunio Paulo Crasso Patavino accuratissime in latino sermone versi. Padua, Frambotti, 1700.
9Galeno: Adscripti libri. Venice, Valgrisium, 1562.
10Aetius of Amida: Librorum medicorum tomus primum; in Manutii A, Asulani A: Aedibus Aeredum. Venice,